Maximising innovation opportunities in digital medicine
Digital medicine is a vast discipline encompassing many interconnected elements. It’s also growing and evolving at pace as the sophisticated technologies behind it become more affordable and accessible. A Global Market Insights report published in March 2023 projects that the wider digital health market will experience a Compound Annual Growth Rate (CAGR) of 15% between 2023 and 2032, to reach USD 981.5 Billion.
The term ‘digital medicine’ is perhaps overused, covering a wide range of health-related digital technologies. At Sagentia Innovation, we adhere to the definition centred on “evidence-based solutions that use software and algorithmically driven products to measure or intervene to improve human health.”
From a patient perspective, this is about health promotion and disease prevention. From a wider healthcare perspective, it’s about supporting health research and the practice of medicine.
Whatever definition you use, innovation prospects within this fertile landscape are immense. Digital medicine offers ways to improve patient experiences and outcomes while making healthcare systems more effective and efficient. It also presents opportunities to drive the transition from ‘sick care’ to true ‘health care’, empowering people to maintain good health and facilitating earlier interventions to prevent illness.
Yet the vast, complex, and dynamic nature of digital medicine can make it hard to identify technically feasible and commercially viable concepts.
To help companies navigate this exciting and potentially lucrative space, we’ve created a Digital Medicine Landscaping Tool. It’s an interactive taxonomy of digital medicine which encompasses measurement and intervention cycles for a comprehensive range of prevention, detection, and intervention episodes. It details patient need, intervention function, and enabling classes of technologies which measure and leverage data to enable care. The goal is to map the opportunity space at a high level for rapid evaluation and roadmap planning by R&D teams.
Benefits of the Digital Medicine Landscaping Tool
Patient pathways run through the tool, and it is designed to facilitate patient-centric solutions. It identifies measurement-intervention cycles to satisfy various objectives such as providing reassurance, minimising central hospital visits, reinforcing healthy behaviours, and more.
Companies already active in digital medicine can use the tool to audit current solutions and identify opportunities to add further value in specific areas. An existing diagnostic solution for at-home use might be enhanced to offer patients prevention lifestyle guidance. Or healthcare professionals might be empowered with new intervention capabilities via procedure monitoring and planning to support evidence-based treatment and best practice.
For R&D teams developing new digital medicine solutions, the tool makes it easier to identify a greater range of potential measurement-intervention concepts early in the design process. This allows more ideas to be hypothesised and interrogated upfront, with the strongest progressed for development.
Identifying enabling technologies
The tool also aids the identification of enabling technologies which can be combined in different ways to deliver value according to defined needs and objectives. They are grouped into five overarching categories:
- Data sources – these technologies produce digital information via the front-end collection of data, measurement of raw data and detection of biomarkers. They include wearable sensors and edge detection devices, in vitro diagnostics, medical imaging systems, drug delivery devices, and simple manual reporting (e.g. logging symptoms or events).
- Data management – technologies in this category enable the safe and efficient storage, aggregation, and flow of data. Examples range from ‘top down’ tools such as central, local, or cloud-based systems for electronic medical records to ‘bottom up’ solutions for personal health records maintained by the individual, like Apple’s HealthKit.
- Visualisation – the way descriptive and predictive information is presented plays a key role in digital medicine. This can be handled via web-based stakeholder portals, customised displays, devices such as smartphones and tablets for on-the-move data, and augmented reality tools which increasingly provide richer, context specific information.
- Decision support – tools that assist prescriptive action from complex data are a critical enabler. They use models to abstract complex aggregated data to generate new knowledge, helping stakeholders rapidly absorb and act upon relevant information, for instance via simple trending or risk scores. Examples include insulin bolus calculators or cardiac risk scores from remote ECG data.
- Interoperability – technologies such as Bluetooth LE, cellular, and ethernet are fundamental to digital medicine, enabling connectivity between end-to-end elements. The protocols which govern them, such as HL7 and continua, are another crucial element, allowing integration of data sources and data management systems from various manufacturers as they operate across different platforms.
The Digital Medicine Landscaping Tool makes it easier for developers to determine which technology classes can perform necessary functions to meet specific patient needs. This aids the creation of digital medicine development roadmaps for individual devices, and their integration with – or enablement of – wider digital medicine ecosystems.
Supporting digital medicine roadmap development
When digital medicine is applied to specific aspects of a given health issue, it generates new seams of data which inform further analysis and research. This in turn delivers deeper insights which can be used to improve disease management, treatment outcomes, and population health trends.
Type 2 diabetes is a case in point. A core patient need is the regular monitoring of blood glucose levels, a function traditionally performed using the finger-prick blood test. Giving this analogue method a digital medicine overhaul can unlock significant benefits at the individual and populational level.
The digital medicine landscape for type 2 diabetes
Continuous Glucose Monitoring (CGM) is emerging as a modern data source, allowing individuals to visualise and track blood glucose levels in real-time, and enabling remote patient monitoring. The ‘monitoring treatment efficacy’ slice of the intervention segment of the Digital Medicine Landscaping Tool reveals further technology classes that could be leveraged to deliver additional benefits.
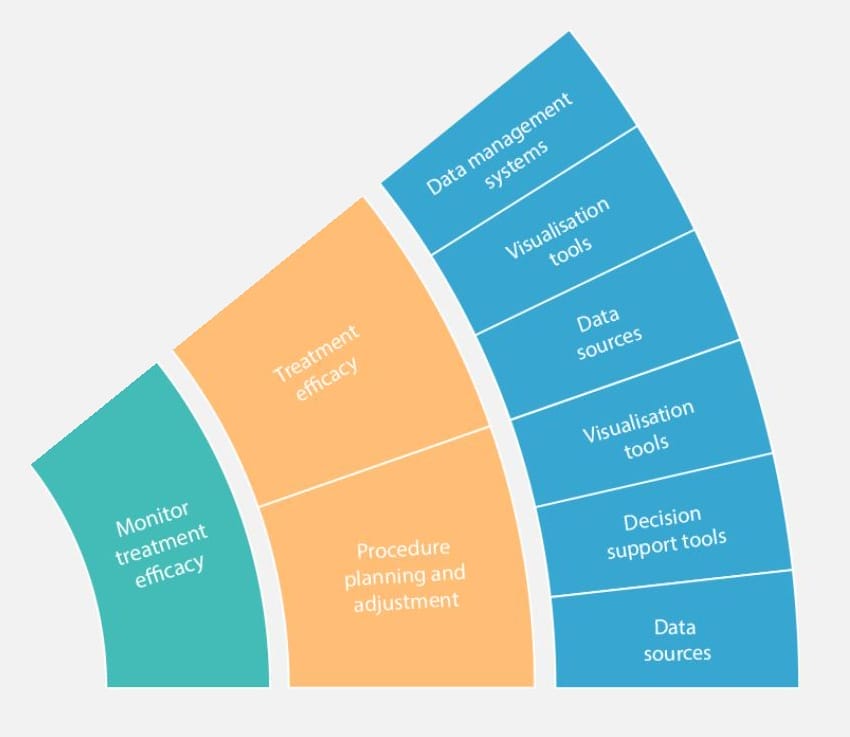
For instance, data management systems combined with relevant interoperability technologies would allow blood glucose information to be shared meaningfully with healthcare providers. This in turn facilitates targeted ‘procedure planning and adjustment’ using clinical decision support tools. Digital, intervention delivery devices such as smart pens and patches come into play here, managing insulin administration and dosage tracking.
Together, these technology enablers could form the basis for addressing wider therapeutic needs of people with type 2 diabetes. Or they could facilitate expansion into the realm of prophylactic treatment for those at risk of developing the illness.
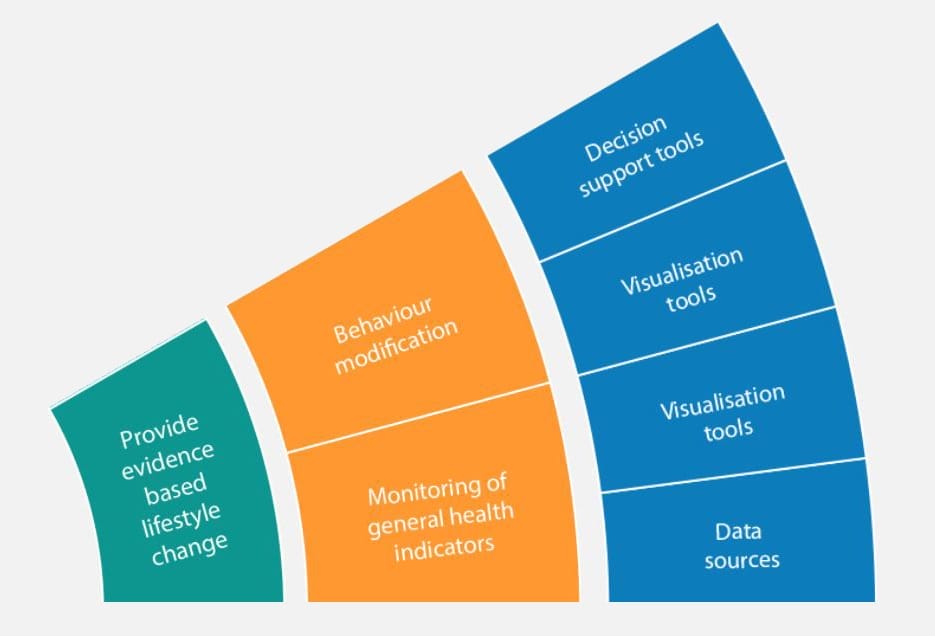
A prevention digital medicine solution for type 2 diabetes might centre on improving diet or providing evidence-based guidance for lifestyle change. Mobile apps plotting blood glucose level trends could act as a primary visualisation tool to enable this. Patient self-care (behaviour modification) would be stimulated via dietary recommendations, empowering people with prediabetes to manage their condition more proactively. There is also scope to extend this through mechanisms enabling individual patients to access peer support and reassurance.
Further opportunities lie in the development of strong data management systems and decision support tools leveraging information related to type 2 diabetes at a macro level. Digital data sources result in a richer dataset for diagnostic intervention, as well as enabling the indication of co-morbidities and identification of potential complications.
Large datasets from diverse sources (e.g. genomic, physiometric, and patient lifestyle), enabled by data management systems, hold much potential for type 2 diabetes management. Their analysis facilitates pattern identification, prediction of blood glucose fluctuations, and personalised treatment recommendations, all of which can underpin product opportunities. Visualisation and decision support algorithms can learn from historical data to optimise insulin dosing and alert individuals to potential hypo- or hyperglycaemic events. Even better, prevention digital medicine based on strong decision support tools such as AI or machine learning could identify individuals approaching the tipping point of type 2 diabetes, then contribute to advice on pre-emptive action to avoid it.
Improving human health
Digital medicine leverages digital health data to generate evidence-based solutions for the improvement of human health. It presents opportunities across all application areas for safe, effective, and truly patient-centric approaches.
Products and services developed with digital capabilities have a critical role to play throughout the digital medicine ecosystem, from measurement and intervention to decision support. Our Digital Medicine Landscaping Tool facilitates high-level ideation, showing how different technology classes can address specific clinical functions and patient needs. And our scientists, engineers, technologists, and data specialists can map digital medicine landscapes in greater detail, maximising the innovation opportunity for improved human health and commercial returns. Contact us to find out how we can help you maximise your opportunity in digital medicine [email protected].
Complete the form to view the interactive graphic.
